Nutrition
The Ultimate Guide to Intermittent Fasting (Can It Help With Weight Loss?)
What if skipping breakfast could do more than just save time in the morning? Intermittent fasting has been making waves for its potential to help with weight loss, boost energy, and even improve brain health.
But let’s be real – fasting isn’t one-size-fits-all, and doing it wrong can backfire. So, how do you tap into its benefits without turning into a hangry mess? In this guide, we’ll uncover everything you need to know about intermittent fasting, from choosing the right fasting method to making it work with your body’s unique rhythm.
Table of Contents
Are you fasting or starving? How to start intermittent fasting?
The first rule of intermittent fasting is simple: don’t starve yourself.
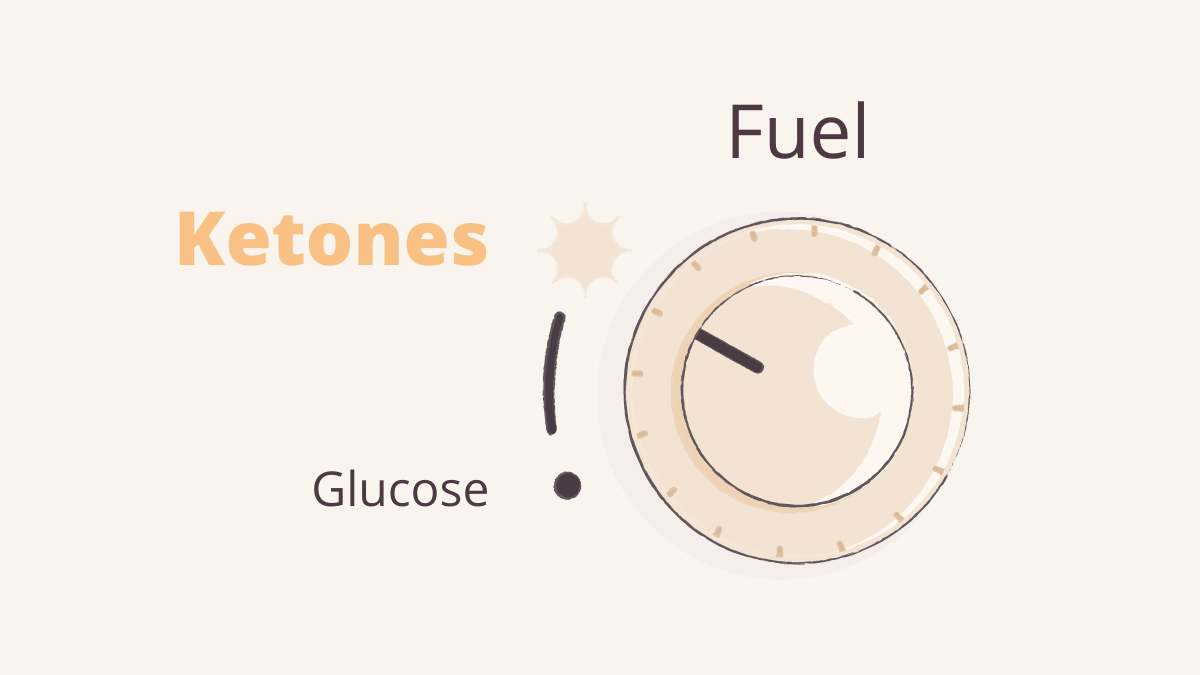
Your body runs on both glucose and fat for energy. While fat provides most of the energy at rest, glucose is vital for certain functions. For example, red blood cells rely entirely on glucose, and at least 33% of your brain’s energy comes from it – even when ketones are available.1 2
On average, your blood contains about 4 grams of sugar, with 60% of it fueling the brain.3 Keeping this balance is essential, as dangerously low blood sugar can disrupt your metabolism or even become life-threatening.
The key to fasting safely? Understand your body’s energy needs and avoid pushing it into starvation mode.
What are the most common fasting methods?
If you’re ready to try intermittent fasting, the 16:8 method is a great place to start. This approach involves fasting for 16 hours and eating within an 8-hour window. It’s easy to stick to and may support weight loss, improve heart health, control blood sugar, and reduce inflammation.4
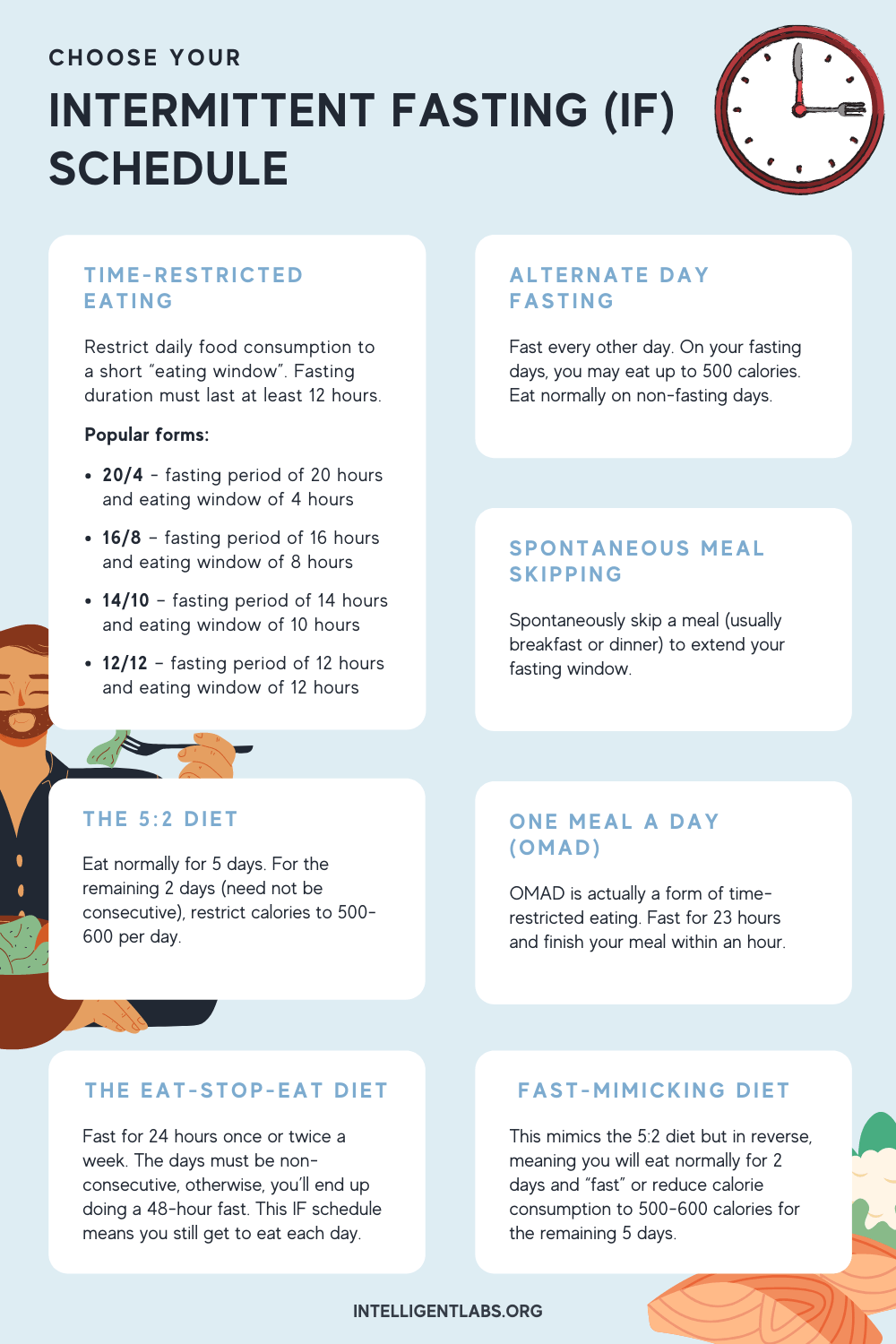
Other popular methods include:
- The 5:2 Diet: Eat normally for five days a week, then limit your intake to 500–600 calories on two non-consecutive days.
- Alternate-Day Fasting: Alternate between regular eating days and days where you restrict your calorie intake to 500–600 calories.
Each method offers similar benefits, so choose the one that best fits your lifestyle.
Check out the infographic below for other intermittent fasting schedules:
Which supplements can support your intermittent fasting journey?
Intermittent fasting can be transformative, but the right supplements can make your journey smoother and more effective. Here are three to consider:
Fasting positively impacts gut microbiota, which supports digestion, immunity, and overall health. Probiotics may help maintain balance in the microbiome, especially during the adjustment phase.5

This essential mineral supports muscle function, energy production, and relaxation. It’s particularly beneficial during fasting to help prevent fatigue, cramps, and sleep disturbances that may arise from electrolyte imbalances.6 7
Early stages of fasting can stress the body, increasing cortisol levels. Phosphatidylserine helps regulate cortisol, reducing stress and supporting a smoother transition.8
Including these supplements in your routine might help you maximize the benefits of fasting while minimizing challenges.
What’s the role of the liver in fasting?
The liver plays a key role in maintaining stable blood sugar during fasting. When blood sugar drops, the brain signals the liver to release glycogen or produce glucose through gluconeogenesis.9 10
Once glycogen stores (about 80–100 grams) are used up, the body shifts to burning fat. The liver converts fatty acids from fat cells into ketones, which serve as an alternative energy source for the brain.
What’s the role of ketones in fasting?
Ketones are your body’s backup fuel during fasting. When glucose levels drop, the liver produces ketones to provide a steady, efficient energy source for the brain.11 12
Unlike fatty acids, which the brain can use minimally, ketones reduce reliance on glucose and prevent excessive stress hormone release, keeping your energy levels stable.
Who should do intermittent fasting?
Intermittent fasting is ideal for people who are physically fit and active. They efficiently produce ketones and easily switch between burning glucose and fat, making fasting feel natural and sustainable.13 14
Who should NOT do intermittent fasting?
Fasting can be difficult for those who are overweight, inactive, or dealing with health issues. These individuals may lack metabolic flexibility – the ability to shift between using glucose and fat for energy – making fasting more stressful and less effective.15 16
So how do I know if I can handle intermittent fasting?
Two warning signs may indicate your body isn’t ready for intermittent fasting:
Warning sign #1: Rapid weight loss
Shedding pounds too quickly, especially water or muscle, is a red flag. Fasting depletes glycogen stores, which are stored with water. To give you an idea, burning 600 grams of glycogen can result in up to 3 kg (6.6 lbs) of water weight loss.17 Muscle breakdown for energy adds to this, leaving you weaker, not healthier.
Warning sign #2: Fasting feels like a struggle
Fasting shouldn’t feel miserable. Symptoms like dizziness, irritability, or intense cravings suggest your body isn’t producing enough ketones to compensate for low glucose. Stress hormones kick in, causing hunger, weakness, mood swings, or anxiety.
If fasting leaves you feeling unwell, it’s a sign to pause and reassess your approach.
If I feel bad, should I avoid intermittent fasting altogether?
Not necessarily! If fasting feels difficult, your body might not be fat-adapted yet, meaning it hasn’t learned to burn fat and produce ketones efficiently.
To prepare, consider following a high-fat, low-carb diet for about three weeks (here’s our guide to help your body get into ketosis easily). This helps your body transition into ketosis, training it to rely on fat for energy and produce enough ketones.
Once fat-adapted, fasting will feel more natural, with fewer side effects like fatigue or cravings.
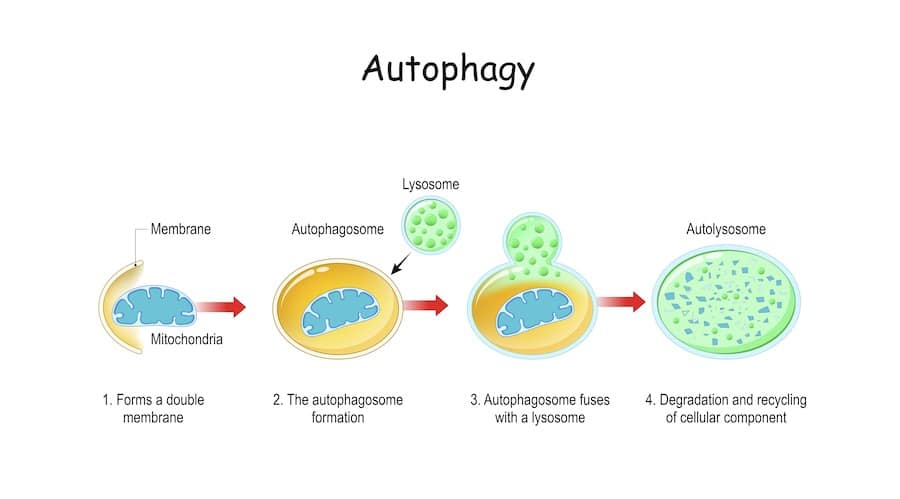
What is autophagy, and how does intermittent fasting trigger it?
Autophagy is your body’s natural cleanup process, recycling old and damaged cells to keep things running smoothly. Think of it as decluttering at the cellular level. This process typically kicks in around 12 hours after your last meal, making the 16:8 method a great way to activate it.18
Autophagy supports improved metabolism, a stronger immune system, and may even slow down aging.
Can you exercise while intermittent fasting?
Yes, exercising while fasting can enhance its benefits, like boosting autophagy.19 However, it’s important to listen to your body.
If you’re fat-adapted, exercise should feel manageable. But if you experience dizziness or extreme fatigue, scale back. Start with low-intensity workouts and gradually increase as your body adjusts.
The key is balance. Exercise should support fasting, not push your body to the limit.
Can children and teens try intermittent fasting?
Intermittent fasting isn’t recommended for kids or teens, especially during puberty, as they need extra nutrients and calories for growth. Skipping meals, like breakfast, can also harm cognitive performance, particularly problem-solving skills.20 21
Young individuals should prioritize a balanced diet and regular meals to support healthy development.
Conclusion
Intermittent fasting can deliver impressive health benefits, including weight loss, better metabolism, and cellular repair. The key is to understand your body’s needs and prepare properly.
Start slow, adapt your diet, and give your body time to adjust. Once you’ve eased into it, intermittent fasting can become a sustainable and effective tool for improving your overall health.
💬 Tried intermittent fasting? Share your experience in the comments below!
📩 Want more diet and wellness tips? Sign up for our newsletter for expert insights and exclusive offers!
References:
- Carnitine transport and fatty acid oxidation, Nicola Longo, Marta Frigeni, Marzia Pasquali, Biochim Biophys Acta . 2016 Oct;1863(10):2422-35. ↩︎
- Biochemistry, Ketone Metabolism, Caleb B. Cantrell; Shamim S. Mohiuddin. StatPearls [Internet]. ↩︎
- Four grams of glucose, David H Wasserman, Am J Physiol Endocrinol Metab . 2009 Jan;296(1):E11-21. ↩︎
- Effects of Time-Restricted Eating on Weight Loss and Other Metabolic Parameters in Women and Men With Overweight and Obesity: The TREAT Randomized Clinical Trial, Dylan A Lowe, Nancy Wu, Linnea Rohdin-Bibby, A Holliston Moore, JAMA Intern Med . 2020 Nov 1;180(11):1491-1499. ↩︎
- Amna Shehbaz, et al. “Intermittent Fasting and Probiotics: Synergistic Modulation of Gut Health for Therapeutic Advantages.” Probiotics and Antimicrobial Proteins, 11 Sept. 2024, https://doi.org/10.1007/s12602-024-10358-5. ↩︎
- National Institutes of Health. “Magnesium.” National Institutes of Health, 2 June 2022, ods.od.nih.gov/factsheets/Magnesium-HealthProfessional/. ↩︎
- Shrimanker, Isha, and Sandeep Bhattarai. “Electrolytes.” National Library of Medicine, StatPearls Publishing, 24 July 2023, www.ncbi.nlm.nih.gov/books/NBK541123/. ↩︎
- Hellhammer, Juliane, et al. “A Soy-Based Phosphatidylserine/ Phosphatidic Acid Complex (PAS) Normalizes the Stress Reactivity of Hypothalamus-Pituitary-Adrenal-Axis in Chronically Stressed Male Subjects: A Randomized, Placebo-Controlled Study.” Lipids in Health and Disease, vol. 13, no. 1, 31 July 2014, https://doi.org/10.1186/1476-511x-13-121. ↩︎
- Some hormonal influences on glucose and ketone body metabolism in normal human subjects, D G Johnston, A Pernet, A McCulloch, G Blesa-Malpica, J M Burrin, K G Alberti, Ciba Found Symp . 1982;87:168-91. ↩︎
- Fundamentals of glycogen metabolism for coaches and athletes, Bob Murray and Christine Rosenbloom, Nutr Rev. 2018 Apr; 76(4): 243–259. ↩︎
- Postexercise muscle glycogen resynthesis in humans, Louise M Burke, Luc J C van Loon, John A Hawley, J Appl Physiol (1985) . 2017 May 1;122(5):1055-1067. ↩︎
- Why does brain metabolism not favor burning of fatty acids to provide energy? – Reflections on disadvantages of the use of free fatty acids as fuel for brain, Peter Schönfeld, and Georg Reiser, J Cereb Blood Flow Metab. 2013 Oct; 33(10): 1493–1499. ↩︎
- Fatty acid and ketone body metabolism in the rat: response to diet and exercise, E W Askew, G L Dohm, R L Huston, J Nutr . 1975 Nov;105(11):1422-32. ↩︎
- POST-EXERCISE KETOSIS R.H. Johnson J.L. Walton H.A. Krebs D.H. Williamson, Published:December 27, 1969 ↩︎
- Dietary restriction and 2-deoxyglucose administration improve behavioral outcome and reduce degeneration of dopaminergic neurons in models of Parkinson’s disease, W Duan, M P Mattson, J Neurosci Res . 1999 Jul 15;57(2):195-206. ↩︎
- Beneficial effects of intermittent fasting and caloric restriction on the cardiovascular and cerebrovascular systems, Mark P Mattson, Ruiqian Wan, J Nutr Biochem . 2005 Mar;16(3):129-37. ↩︎
- Glycogen storage: illusions of easy weight loss, excessive weight regain, and distortions in estimates of body composition, S N Kreitzman, A Y Coxon, K F Szaz, Am J Clin Nutr . 1992 Jul;56(1 Suppl):292S-293S ↩︎
- Flipping the Metabolic Switch: Understanding and Applying the Health Benefits of Fasting, Stephen D Anton, Keelin Moehl… Obesity (Silver Spring) . 2018 Feb;26(2):254-268. ↩︎
- Exercise and exercise training‐induced increase in autophagy markers in human skeletal muscle, Nina Brandt, Thomas P. Gunnarsson, Physiol Rep. 2018 Apr; 6(7): e13651. ↩︎
- Nutrition for the Next Generation: Older Children and Adolescents, Jai K Das, Zohra S Lassi, Zahra Hoodbhoy, Rehana A Salam, Ann Nutr Metab . 2018;72 Suppl 3:56-64. ↩︎
- Fasting and cognitive function, E Pollitt, N L Lewis, C Garza, R J Shulman, J Psychiatr Res . 1982;17(2):169-74. ↩︎




